Understanding Hysterectomy Incontinence Risk: A Comprehensive Guide

When considering a hysterectomy, many women have concerns about potential postoperative complications, especially the risk of hysterectomy incontinence. Understanding this risk, its causes, prevention measures, and the role of experienced Obstetricians & Gynecologists is crucial in making an informed decision about your healthcare. In this comprehensive guide, we delve into the intricacies of hysterectomy incontinence risk, offering valuable insights backed by medical expertise.
What Is a Hysterectomy and Why Is It Performed?
A hysterectomy is a surgical procedure to remove the uterus. It is one of the most common gynecological surgeries performed worldwide and can be recommended for various reasons, including:
- Heavy or abnormal uterine bleeding unresponsive to other treatments
- Uterine fibroids causing pain or discomfort
- Endometriosis
- Pelvic organ prolapse
- Cancerous or precancerous conditions of the uterus or cervix
- Persistent pelvic pain
Despite its effectiveness, a hysterectomy is a major operation with potential risks and long-term implications, among which incontinence is a significant concern that merits attention.
Understanding Hysterectomy Incontinence Risk
What Is Incontinence?
Urinary incontinence refers to the involuntary leakage of urine, which can profoundly affect a woman’s quality of life. It ranges from occasional dribbling to complete loss of bladder control. When discussing hysterectomy incontinence risk, it primarily pertains to stress urinary incontinence (SUI), which occurs when physical activity increases intra-abdominal pressure, leading to urine leakage.
How Does a Hysterectomy Influence Incontinence?
The relationship between hysterectomy and incontinence is complex. Changes in pelvic anatomy, nerve function, and support structures following the surgery can contribute to urinary issues. Significant factors that influence the hysterectomy incontinence risk include:
- Type of hysterectomy performed: Total versus subtotal hysterectomy may have differing impacts on pelvic support.
- Preservation of pelvic floor muscles and ligaments: Adequate preservation or reinforcement reduces the risk.
- Pre-existing pelvic floor weakness or pelvic organ prolapse: Existing conditions heighten vulnerability.
- Nerve damage during surgery: Can impair bladder control mechanisms.
- Age and overall health: Older women or those with comorbidities may have increased risk.
Prevalence and Statistics of Post-Hysterectomy Incontinence
Research indicates that approximately 10-20% of women undergoing hysterectomy experience some form of urinary incontinence postoperatively. While many cases are mild and manageable, a subset of women face persistent or worsening symptoms. Proper surgical planning and postoperative management are essential to mitigate this risk.
Factors Contributing to Hysterectomy Incontinence Risk
Preoperative Factors
Several preoperative factors can influence postoperative outcomes including:
- Existing pelvic floor dysfunction: Women with prior pelvic organ prolapse or prior incontinence have increased risk.
- Severity of uterine or pelvic pathology: Larger fibroids or severe endometriosis may complicate surgery.
- Age and tissue elasticity: Older women with less elastic tissue tend to have higher risk.
Intraoperative Factors
During surgery, the surgeon’s expertise and technique play a pivotal role in minimizing risk:
- Use of meticulous surgical techniques: Preserving pelvic support structures reduces incontinence risk.
- Aware handling of nerves and blood vessels: Prevents nerve damage that could impair bladder control.
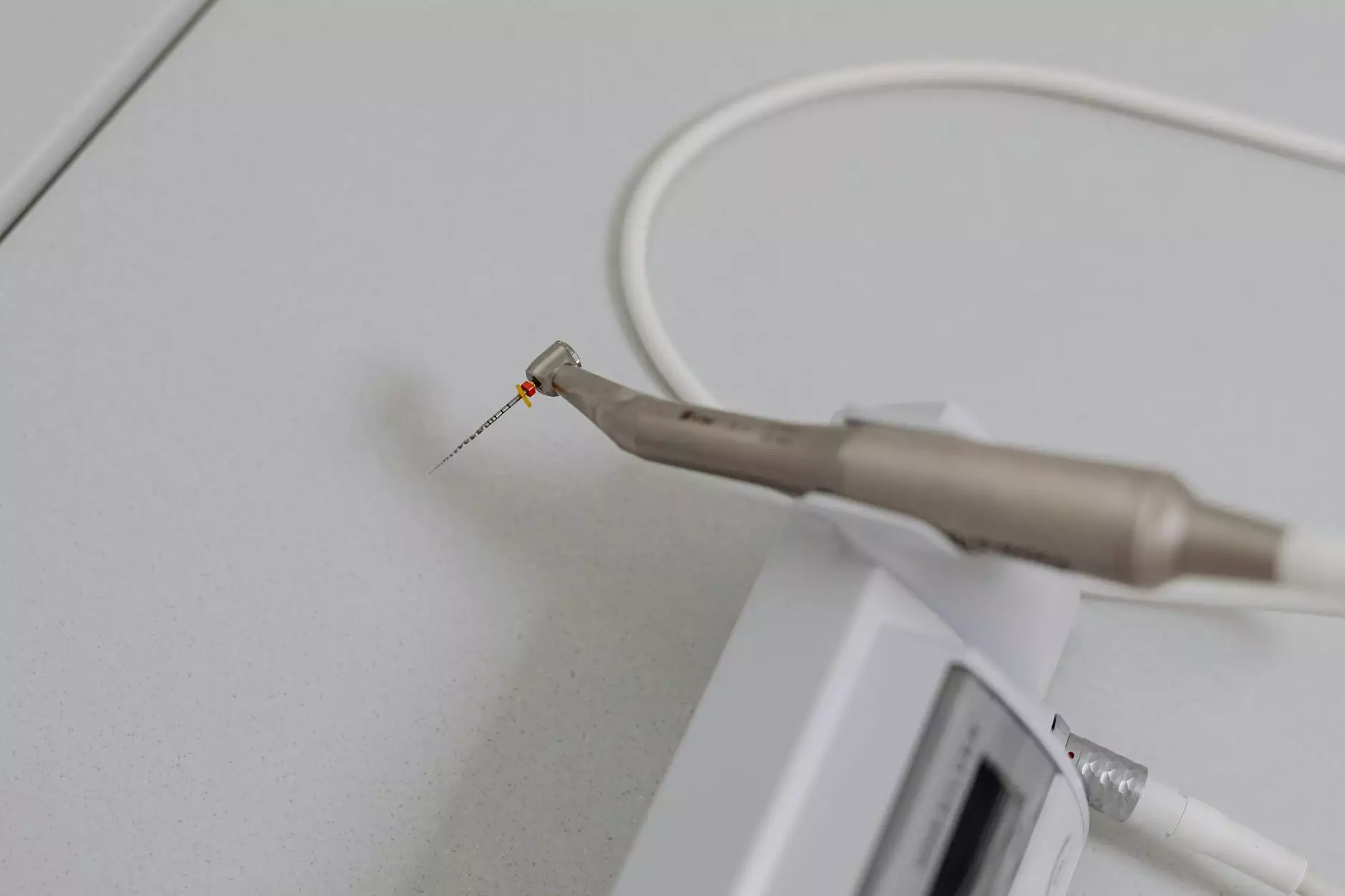
- Type of hysterectomy: Vaginal, laparoscopic, or abdominal approaches carry different risk profiles.
Postoperative Factors
Healing processes and lifestyle choices after surgery influence long-term outcomes:
- Pelvic floor strengthening exercises: Kegel exercises can improve muscle tone and decrease incontinence risk.
- Weight management: Obesity increases intra-abdominal pressure, heightening risk.
- Managing constipation: Prevents undue pressure on pelvic organs.
Preventing and Managing Hysterectomy Incontinence
Preoperative Counseling and Assessment
A comprehensive preoperative evaluation by an experienced Obstetrician & Gynecologist can identify women at higher risk for hysterectomy incontinence. This includes pelvic examinations, urodynamic tests, and addressing existing pelvic floor weakness before surgery.
Choosing the Right Surgical Approach
The choice of hysterectomy method significantly impacts future urinary function. Minimally invasive techniques like laparoscopic or vaginal hysterectomy often preserve pelvic support better and are associated with lower incontinence risk. Discussing these options with your surgeon can help tailor the surgery to your specific needs.
Rehabilitation and Lifestyle Modifications
Postoperative rehabilitation programs, including pelvic floor physical therapy, play a vital role in reducing the hysterectomy incontinence risk. Lifestyle measures such as maintaining a healthy weight, quitting smoking, and avoiding bladder irritants are also beneficial.
When Should You Consult a Specialist?
If you experience symptoms like involuntary urine leakage, frequent urination, or feeling of incomplete bladder emptying after hysterectomy, it’s imperative to consult with a specialized Obstetrician & Gynecologist. Early intervention with therapies or surgical options like sling procedures can effectively manage incontinence.
The Role of Expert Gynecologists at drseckin.com
At drseckin.com, our team of highly experienced Obstetricians & Gynecologists specialize in advanced gynecological surgeries with a focus on minimizing hysterectomy incontinence risk. We prioritize personalized treatment plans, utilizing state-of-the-art minimally invasive techniques, and providing comprehensive pre- and post-operative care to ensure optimal outcomes for our patients.
Summary: Making an Informed Decision About Hysterectomy
While the hysterectomy incontinence risk is an important consideration, advancements in surgical techniques and preoperative assessment have significantly reduced its occurrence. Understanding the risk factors, choosing skilled surgeons, and adhering to postoperative recommendations can greatly influence your recovery and long-term well-being.
The Importance of Expert Medical Guidance
To truly understand your personal hysterectomy incontinence risk and explore suitable surgical options, consult with a qualified Obstetrician & Gynecologist. At drseckin.com, we are committed to guiding women through every step of their gynecological health journey with compassion, expertise, and cutting-edge care.
Remember, informed decisions and proactive management are key to maintaining a healthy, confident life post-hysterectomy.